You’ve probably already heard about the benefits of digital transformation in Healthcare and read even more times about what an important trend this is. But very few talk about the pitfalls with data, compliance with regulations and, in general, about the process of implementing this very digitalization in medical companies and hospitals.
Therefore, in this article we will touch on the positive aspects through the prism of the problems that companies may face.
Digital healthcare includes a variety of medical services:
- information technology (IT);
- mobile healthcare (mHealth);
- telemedicine;
- wearable devices;
- EMR;
- AR/VR;
- blockchain;
- personalized treatment services.
And these are just a few examples.. Therefore, now quite a lot of new players have come to this market. According to Global Healthcare Analytics Market forecasts, the cumulative annual growth rate of the global digital healthcare market (CAGR) will be 27.9% in the period from 2020 to 2027, when it will reach more than 90 billion dollars.
Why has digitalization become popular?
Innovations in the field of digital healthcare:
- save time and financial resources of companies;
- improve the accuracy and effectiveness of disease detection;
- eliminate errors when working with data and minimize legal problems.
Let’s talk about this in more detail.
What problems does Digital Transformation solve in Healthcare
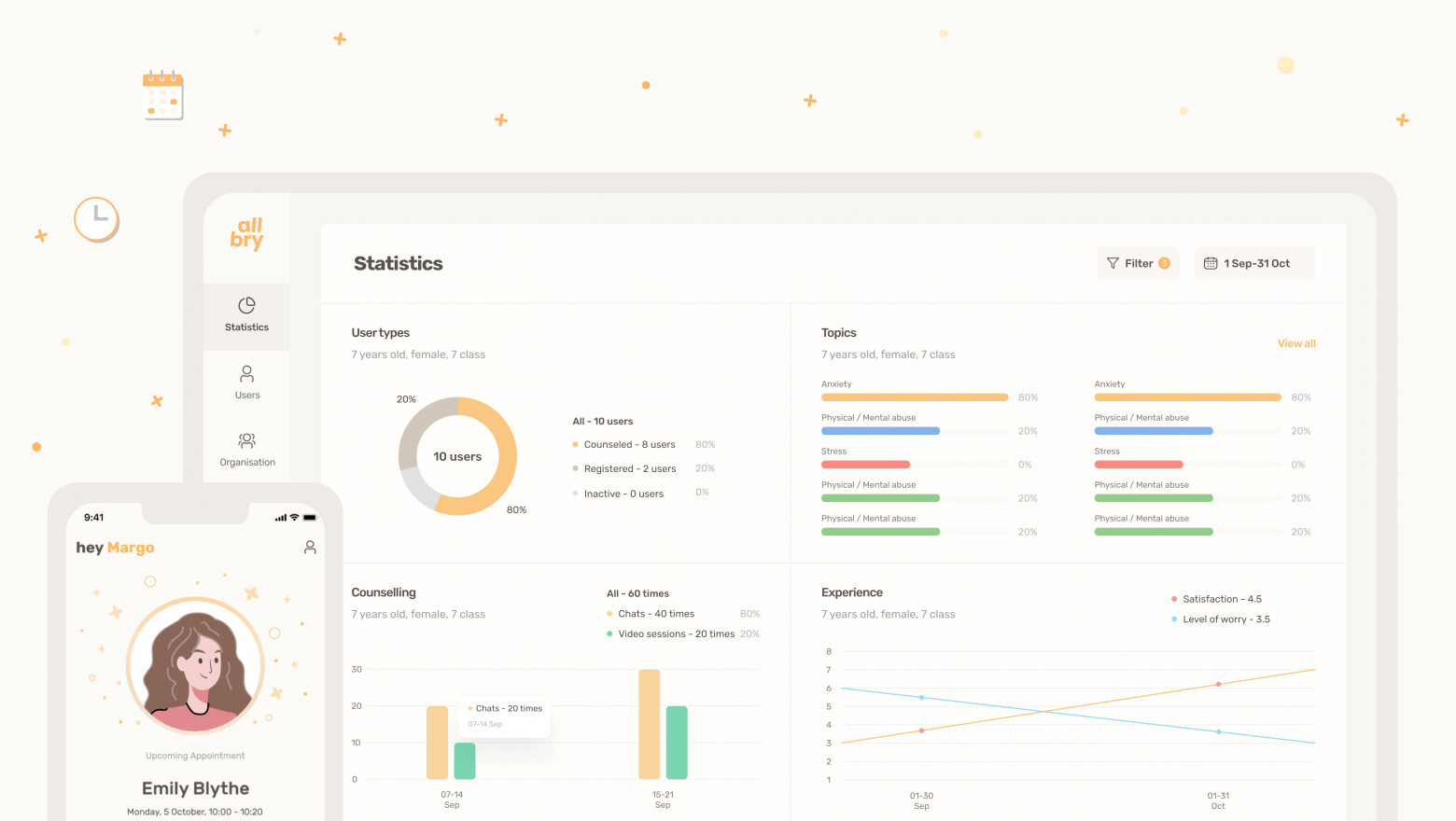
1. Time optimization: communication between the patient and the clinic/doctors
Let’s illustrate this outcome with one situation: Joe, who lives in a small town, had to book his appointment with a doctor no earlier than a month ahead. And all in order to clarify one small question that he forgot to ask during the first consultation. Ridiculous, isn’t it? Now imagine if you have a complication, but there is no quick connection with the right doctor.
Digitalization in clinics can lead to a reduction in the administrative burden on medical workers and other repetitive aspects of their work. This increases their time for actual contact with the patient.
This is especially important for patients or clinics located in rural areas, or for home care, when travel is difficult or not recommended. Thanks to clinical-level technologies, patients can provide information about their health to their doctor at any time.
For example, Zocdoc is a popular healthcare application that allows patients to urgently find a doctor, schedule online video visits at a convenient time and track their annual checkups effortlessly.
2. Monitoring of symptoms and treatment of chronic diseases
Digital healthcare has the potential to prevent diseases and reduce healthcare costs by helping patients control and treat chronic diseases. It can also adapt medications for individual patients.
Thus, personalization and permanent treatment are achieved while reducing total time and money resources. This is a particularly important point, since WHO estimates that by 2035 the global shortage of qualified medical workers will amount to 12.9 million. This creates the need to manage human resources more efficiently.
An example would be Resmed, which tracks sleep apnea using a medical device connected to the cloud.
3. Cost reduction through multi-channel information
Our marketer says that he can “invent” the most terrible diseases for himself and sometimes gets confused about the symptoms. Before making an appointment with a doctor, he discusses his symptoms on various forums and only then understands when it is best to make an appointment.
Digitalization aims to optimize the financial hours of call center employees: create tests that allow patients to be segmented by symptoms. This is necessary to understand which doctor should be contacted next.
There is also a popular trend towards the possibility of using chats in which there are people with similar diseases and who can give advice.
An excellent example of using patient portal technology is the FollowMyHealth system. It allows patients to easily share their medical data.
4. Troubleshooting and task automation
Our friend Carl told us that during his last visit to the trichologist, he spent no less than 20 minutes just filling out papers.. He wondered why an experienced specialist could not ask for an assistant to help or… use a computer to fill in the required data.
Doctors oftentimes spend less than 30% of their time treating patients. Instead, they may spend a better part of an afternoon handling various administrative tasks, such as filling in data into an electronic medical records system.
In a digitalized clinical ecosystem, these tasks can be easily automated with bots that send and sort information without any human involvement.
This helps exclude the human factor that may lead to errors and incorrect calculations. A great example of positive digitalization is Viz.ai. It is helping medical teams to react faster and make decisions about primary care with the help of medical solutions based on artificial intelligence.
5. Data security
Digital data may be at risk of malicious attacks or be deleted/changed due to employee negligence.
With a specially designed digital data storage system, these factors can be eliminated from the equation for medical records. Not only that, authorized personnel can access these records anywhere, ensuring timely availability if necessary. Appropriate security measures ensure that the data remains intact and will not be affected by negligence, natural disasters and so on.
Big data can reduce the frequency of errors when taking medications. Thanks to the analysis of patient records, the software can detect any inconsistencies between the patient’s state of health and the prescription of medications. It then warns healthcare professionals and patients about the potential risk of medication errors.
The same applies to personnel analysis. Big data predictive analysis can help hospitals and clinics assess future admission rates, which will help these institutions allocate the appropriate staff to work with patients. This saves money and reduces the waiting time in the emergency department when there are not enough staff in the institution.
On the other hand, theory sounds good, which is not always the case for practical application.
The above-mentioned advantages may not be achievable due to the complex implementation of the digitalization tools.
Difficulties
1. Digital literacy
The most obvious barrier: many health care consumers lack digital skills, and some even need help creating an email account. Probably you yourself have relatives who have experienced difficulties with this. Therefore, the creation of patient portals, medical trackers, remote monitoring devices, tools for self-management of diseases and recovery may be too complicated for users.
Solution: study the best UI/UX practices in the industry and adapt them respectively. This will not solve the problem 100% if users do not know how to use a smartphone at all, but at least reduce the entry threshold and reduce the number of lost leads.
2. Lack of understanding of “Why”
You should not blindly follow the trend if you do not understand what problem you want to solve with the help of digital transformation. Many healthcare organizations are still facing significant challenges in this area and are starting to implement digital solutions before the assessing the problem that needs to be addressed.
Solution: stop and think again why you need this digital tool and consult with developers who have relevant experience. If your software development partner starts pitching their digitalization services to you intensively without understanding the core problem, start looking for a new provider.
3. Legal subtleties and compliance with standards/laws
The most dangerous point. Due to the massive volumes of data collected from different systems that are stored and encoded differently, data compatibility is an ongoing problem.
From a technical standpoint, several good practices can be incorporated to provide users with the highest level of protection. One of them is using the End-to-end encryption (E2EE) method: only the users actually involved in communication can obtain information. Another common procedure is implementing multi-factor authentication (MFA) to create an additional layer of protection. This way, users can only access their accounts after delivering at least two pieces of personal information, which minimizes the risk of breaches and data leaks.
When it comes to legal aspects that need to be taken into account, it boils down to being compliant with regulations and directives in force in particular regions of the world. Depending on the geographical location and targeted markets, healthcare providers follow different sets of rules. For the United States, it’s The Health Insurance Portability and Accountability Act of 1996 (HIPAA), for Canada — Personal Information Protection and Electronic Documents Act (PIPEDA), and the inhabitants of European Union countries need to comply with GDPR guidelines.
Additional problems are related to ethics. For instance, If you use a device that tracks a chronic illness, then who is responsible for the system failure and further improper treatment: the hospital that received the technology, the developer or the doctor who recommended it?
It might be difficult to keep track of all these healthcare laws. It is even more challenging to apply them to product development and market-specific design.
The main reason many companies fail at the legal point is the lack of experience, which leads to:
– sanctions from government agencies for improper enforcement of the law (for example, they forgot to set up automatic deletion of data in chats, which should be in place according to GDPR);
– budget overruns and longer time to market (if there is no proven model or expert).
Solution: work with a highly specialized partner who has proved use cases and experience in the field. The most acceptable option would not be outsourcing but cooperation with a health product partner, since unlike other formats, you get not just a ready-made solution based on a technical task, but a development with an emphasis on consulting and experience in industry. This way, it is possible to neutralize the risks associated with ignorance of legal issues in Healthcare and lack of experience in adapting standards to UX.
In fact, this is a kind of closed type of interaction with health products, in which wishes are taken into account, but proposals that are not suitable for the market are criticized. Instead, at each iteration of development, ready-made examples and paths are given from which you can choose the next stages of work.
4. Access to technology
In cities, this will be less of a problem. But for the population of rural areas, going online can be become a real roadblock towards accessing digital healthcare due to lack of Wi-Fi or poor communication. One of our clients living in a small village was even unable to reach out to an ambulance because of poor connection, not to mention having online consultation. In this case, you understand how difficult it is to create innovations for remote places.
Also, do not forget about the price of the devices: will the low-income population be able to afford them? Some do not have a smartphone or have one per the entire household which will inevitably lead to problems with data privacy.
5. Product personalization
Mass-produced products may not be suitable for absolutely every company/clinic, as they must be tailored to a specific context and needs.
Solution: opt for custom development, preferably with full immersion of developers in the context to exclude errors.